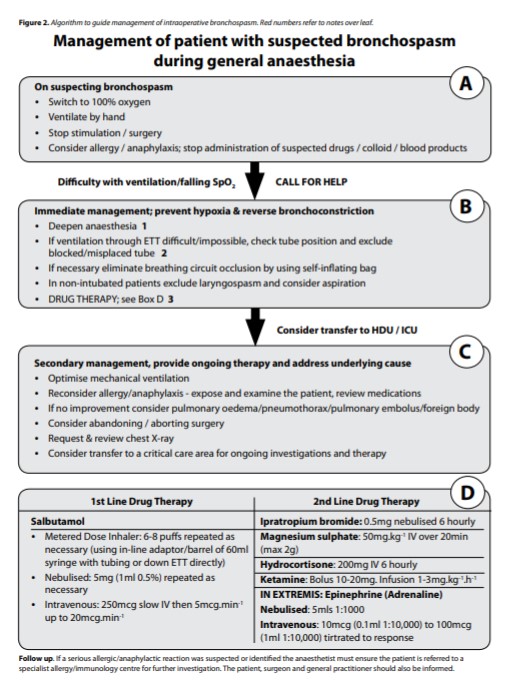
Looseley A. Management of bronchospasm during general anaesthesia. Update in anaesthesia. 2011;27(1):17-21.
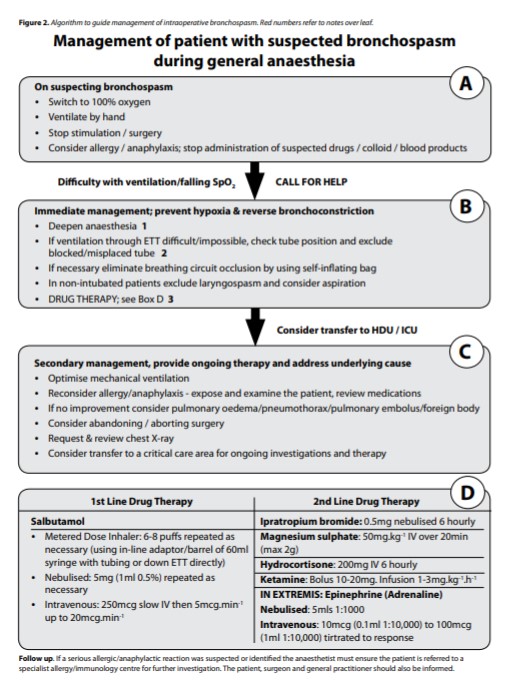

Looseley A. Management of bronchospasm during general anaesthesia. Update in anaesthesia. 2011;27(1):17-21.
Taghavi S, et al. Comparison of open gastrostomy tube to percutaneous endoscopic gastrostomy tube in lung transplant patients. Ann Med Surg (Lond). 2015 Dec 23;5 :76-80.
Introduction: Lung transplant patients require a high degree of immunosuppression, which can impair wound healing when surgical procedures are required. We hypothesized that because of impaired healing, lung transplant patients requiring gastrostomy tubes would have better outcomes with open gastrostomy tube (OGT) as compared to percutaneous endoscopic gastrostomy tube (PEG).
Continue readingBouguen G, et al.; GETAID. Efficacy and Safety of Tumor Necrosis Factor Antagonists in Treatment of Internal Fistulizing Crohn’s Disease. Clin Gastroenterol Hepatol. 2020 Mar; 18(3):628-636.
Results: After a median follow-up period of 3.5 years, 68 patients (43.6%) underwent a major abdominal surgery. The cumulative probabilities for being surgery-free were 83%, 64%, and 51% at 1, 3, and 5 years, respectively. A concentration of C-reactive protein >18 mg/L, an albumin concentration <36 g/L, the presence of an abscess at the fistula diagnosis, and the presence of a stricture were associated independently with the need for surgery. The cumulative probabilities of fistula healing, based on imaging analyses, were 15.4%, 32.3%, and 43.9% at 1, 3, and 5 years, respectively. Thirty-two patients (20.5%) developed an intestinal abscess and 4 patients died from malignancies (3 intestinal adenocarcinomas). One patient died from septic shock 3 months after initiation of anti-TNF therapy.
Conclusions: In a retrospective analysis of data from a large clinical trial, we found that anti-TNF therapy delays or prevents surgery for almost half of patients with CD and luminal fistulas. However, anti-TNF therapy might increase the risk for sepsis-related death or gastrointestinal malignancies.
Continue readingClinical diagnosis of brain death: Prerequisites and criteria (UpToDate – login required.)
| Prerequisites |
| Clinical or neuroimaging evidence of an acute central nervous system (CNS) catastrophe (eg, traumatic brain injury, subarachnoid hemorrhage) Exclusion of complicating medical conditions that may confound clinical assessment (no severe electrolyte, acid-base, endocrine, or circulatory [ie, shock] disturbance) No drug intoxication or poisoning, including any sedative drug administered in hospital, which may confound the clinical assessment Core temperature >36°C (97°F) Systolic blood pressure >100 mmHg; vasopressors may be required |
| Examination findings |
| Coma Absent brain-originating motor response, including response to pain stimulus above the neck or other brain-originating movements (eg, seizures, decerebrate or decorticate posturing) Absent pupillary light reflex; pupils are midposition (3.5 to 4 mm) Absent corneal reflexes Absent oculocephalic (doll’s eyes) and oculovestibular reflexes (caloric responses) Absent jaw jerk Absent gag reflex Absent cough with tracheal suctioning Absent sucking or rooting reflexes (in neonates) Apnea as demonstrated by apnea test |
| Observation period |
| At least 6 hours; longer time periods recommended in children and for certain conditions such as after cardiac arrest |
Thanks to LeslieAnn S. Kao, MD (General Surgery PGY-4) for suggesting this topic.
Somagutta MR, et al. Euglycemic Diabetic Ketoacidosis and Sodium-Glucose Cotransporter-2 Inhibitors: A Focused Review of Pathophysiology, Risk Factors, and Triggers. Cureus. 2021 Mar 3;13(3):e13665.
The underlying mechanism is mainly enhanced lipolysis and ketone body reabsorption. SGLT2i also stimulates pancreatic alpha cells and inhibits beta cells, causing an imbalance in glucagon/insulin levels, further contributing to lipolysis and ketogenesis. Most patients were diagnosed with blood glucose less than 200 mg/dL, blood pH <7.3, increased anion gap, increased blood, or urine ketones. Perioperative fasting, pancreatic etiology, low carbohydrate or ketogenic diet, obesity, and malignancy are identified precipitants in this review. As normoglycemia can conceal the underlying acidosis, physicians should be cognizant of the EDKA diagnosis and initiate prompt treatment. Patient education on risk factors and triggers is recommended to avoid future events.
Continue readingBrady JT, Kendrick DE, Barksdale EM, Reynolds HL. The Ladd Procedure for Adult Malrotation With Volvulus. Dis Colon Rectum. 2018 Mar;61(3):410.
“Intestinal malrotation is a rare condition that develops during fetal development because of incomplete intestinal rotation or a lack of intestinal rotation around the superior mesenteric artery. Presentation in adulthood, in general, is abnormal and presentation with volvulus is rare. We demonstrate an open Ladd procedure with inversion appendectomy and reduction of paraduodenal hernia of an adult with malrotation with volvulus.”
Havens JM, Columbus AB, Olufajo OA, Askari R, Salim A, Christopher KB. Association of Model for End-Stage Liver Disease Score With Mortality in Emergency General Surgery Patients. JAMA Surg. 2016 Jul 20;151(7):e160789. doi: 10.1001/jamasurg.2016.0789.
Results: A total of 13 552 EGS patients received critical care; of these, 707 (5%) (mean [SD] age at hospital admission, 56.6 [14.2] years; 64% male; 79% white) had CLD and data to determine MELD score at ICU admission. The median MELD score was 14 (interquartile range, 10-20). Overall 90-day mortality was 30.1%. The adjusted odds ratio of 90-day mortality for each 10-point increase in MELD score was 1.63 (95% CI, 1.34-1.98). A decrease in MELD score of more than 3 in the 48 hours following ICU admission was associated with a 2.2-fold decrease in 90-day mortality (odds ratio = 0.46; 95% CI, 0.22-0.98).
Conclusions and relevance: In this study, MELD score was associated with 90-day mortality following EGS in patients with CLD. The MELD score can be used as a prognostic factor in this patient population and should be used in preoperative risk prediction models and when counseling EGS patients on the risks and benefits of operative intervention.
Commentary: Zarrinpar A. Mind MELD or Ignore It at Your Peril. JAMA Surg. 2016 Jul 20;151(7):e160839. doi: 10.1001/jamasurg.2016.0839.