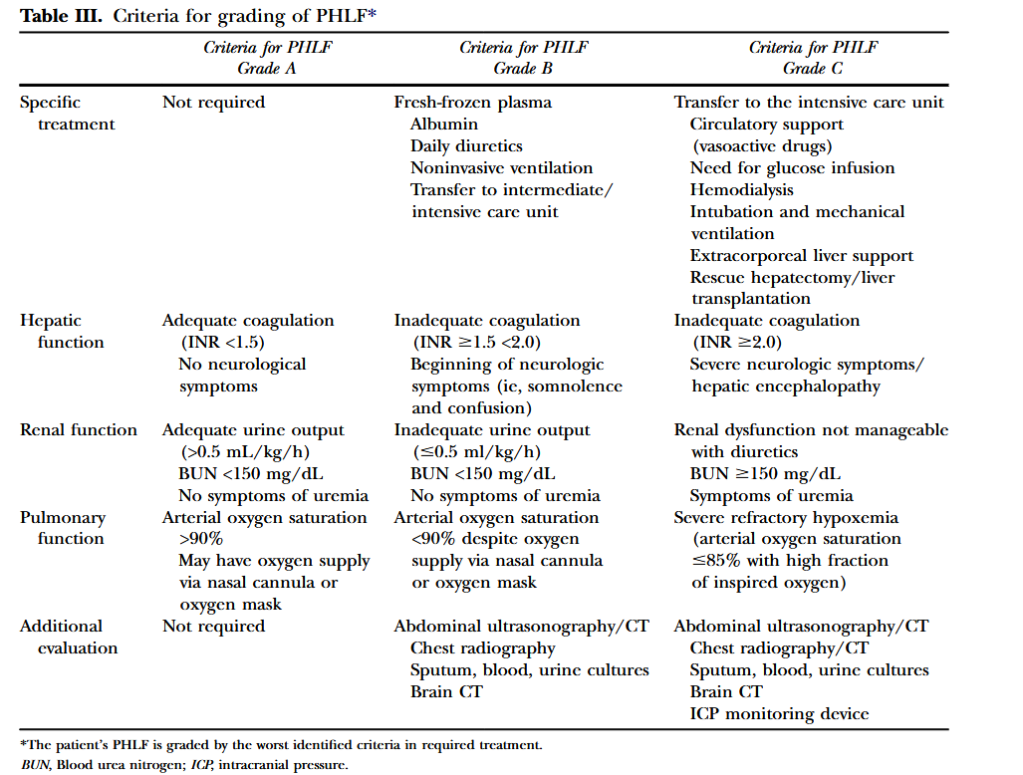
“Liver resection is used increasingly for the management of a variety of benign and malignant conditions. These data have paralleled substantial advances in perioperative management and operative techniques that have improved the safety of, and extended the indications for, liver resection over the past 2 decades. Extended liver resections, liver resections in diseased liver or liver parenchyma affected by chemotherapy, and repeat
or staged liver resections are being used to achieve curative resection and extend long-term survival. The resulting small functional remnant liver volumes and compromised liver function in these patients increase the risk for the development of posthepatectomy liver failure (PHLF). Despite the introduction of functional and imaging measures to assess preoperatively the size and function of the future liver remnant, as well as the use of
portal vein embolization as a preventive intervention, PHLF remains a major concern and has been shown to be a predominant cause of hepatectomy-related mortality.”