“In surgery, adverse events and medical errors occur pre-operatively, intraoperatively, and postoperatively. Standardized classification of postoperative complications, for example, using the Clavien-Dindo classification, is widely adopted, and has proven relevant to research and quality improvement programs. Prospectively validated classification systems for intraoperative adverse events (iAEs) are not yet broadly adopted. IAEs have a major impact at many levels. First, there is an association between iAEs and postoperative outcome. Second, hospital stays for patients experiencing iAEs are 40% more expensive compared with patients without iAEs. Third, readmission rates in patients whose surgery is
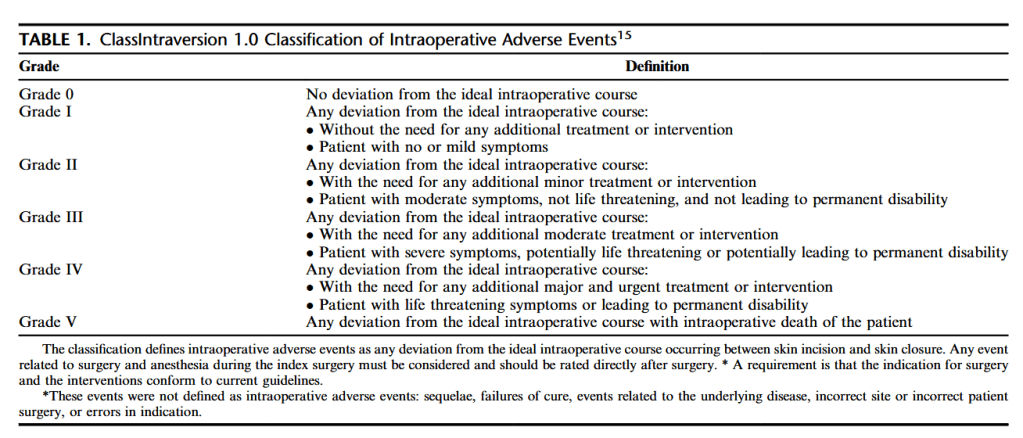
complicated by an iAE are twofold higher. Recently a promising new and practical classification system for iAEs was proposed, the classification of intraoperative complications (CLASSIC). CLASSIC defines iAEs as any deviation from the ideal intraoperative course occurring between skin incision and skin closure, irrespective of the origin (ie, surgical and anesthesiological difficulties, or technical failures). Compared with previous scores such as the severity score by Kaafarani et al. ClassIntra is more inclusive,
accounting for any type iAE, for example, surgical, anesthesiologic, and organizational, and can be graded directly after skin closure.”