“Congenital choladocal cysts are generally treated by resection of the dilated extrahepatic biliary duct followed by hepaticojejunostomy, but it is associated with postoperative complications, including postoperative cholangitis, intrahepatic calculi, pancreatitis, and carcinogenesis, in the remnant bile duct. We investigated the most common long-term complications and identified the factors implicated in their development.”
Continue readingCategory Archives: Hepato-Biliary-Pancreatic
Pancreatitis after Biliary Tract Surgery (Historical article)
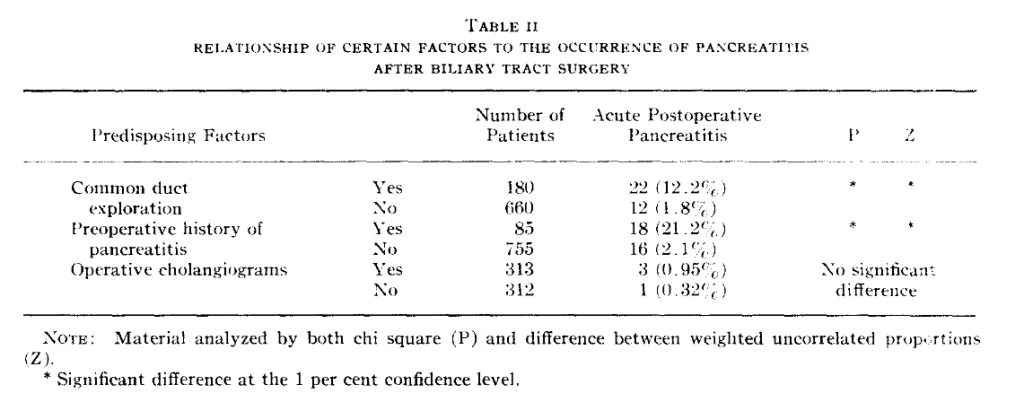
“Acute pancreatitis after operation on the biliary tract is a serious complication. This study was undertaken in an attempt to determine predisposing factors which might exist in patients undergoing operation for biliary tract disease. A large number of patients have been studied by postoperative serum amylase determinations and correlations have been made between the performance of various procedures and the occurrence of clinical and subclinical pancreatitis.”
Posthepatectomy liver failure: A definition and grading by the International Study Group of Liver Surgery (ISGLS)
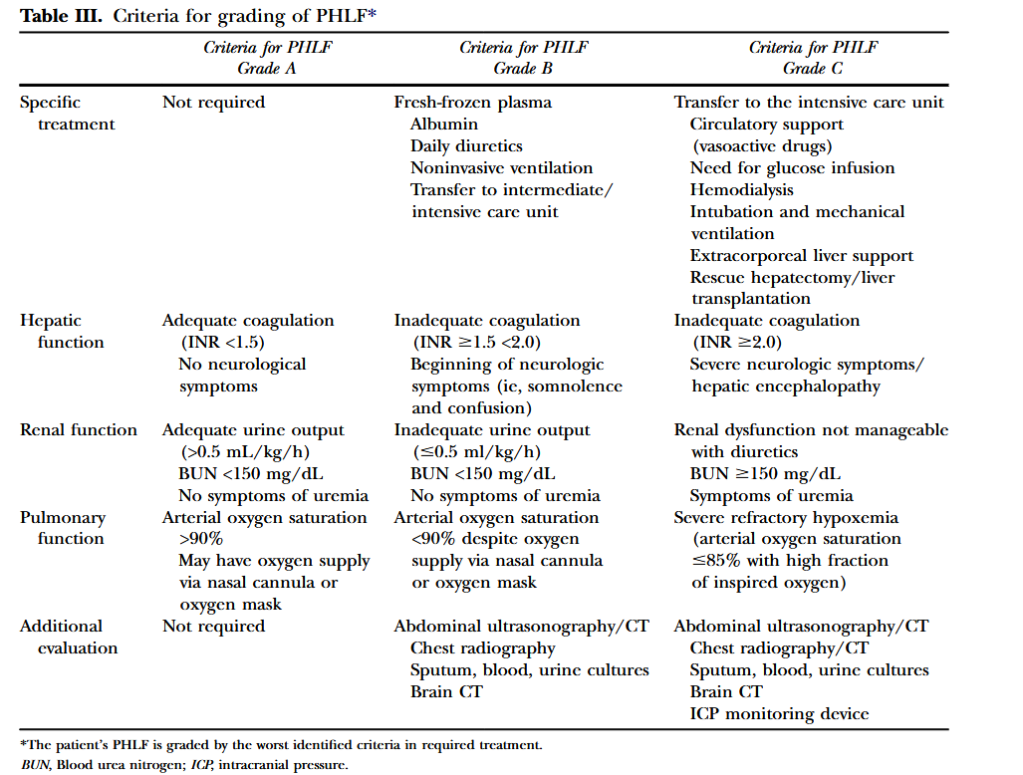
“Liver resection is used increasingly for the management of a variety of benign and malignant conditions. These data have paralleled substantial advances in perioperative management and operative techniques that have improved the safety of, and extended the indications for, liver resection over the past 2 decades. Extended liver resections, liver resections in diseased liver or liver parenchyma affected by chemotherapy, and repeat
or staged liver resections are being used to achieve curative resection and extend long-term survival. The resulting small functional remnant liver volumes and compromised liver function in these patients increase the risk for the development of posthepatectomy liver failure (PHLF). Despite the introduction of functional and imaging measures to assess preoperatively the size and function of the future liver remnant, as well as the use of
portal vein embolization as a preventive intervention, PHLF remains a major concern and has been shown to be a predominant cause of hepatectomy-related mortality.”
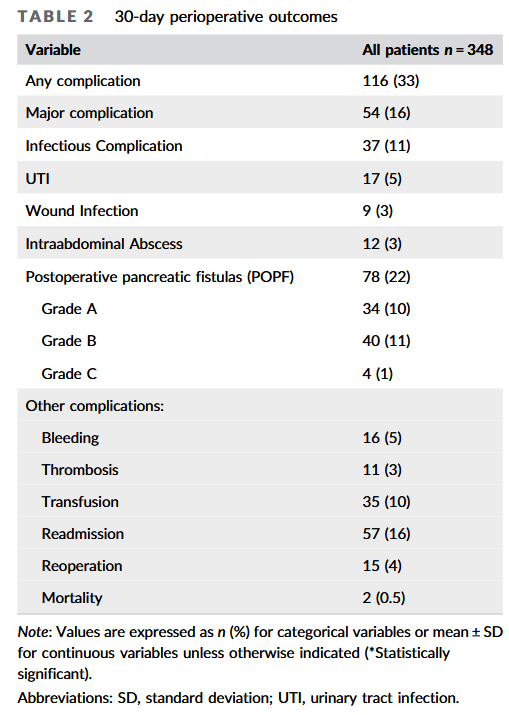
Implications of leukocytosis following distal pancreatectomy splenectomy (DPS) and association with postoperative complications
“Distal pancreatectomy with splenectomy (DPS) is performed to remove pathology of the body and/or tail of the pancreas. The spleen and the left side of the pancreas share blood supply, and often tumor involvement, thus splenectomy is often performed along with distal
pancreatectomy. DPS is an operation that carries a greater than 30% risk of postoperative complications, including infection, postoperative pancreatic fistula (POPF), intraabdominal abscesses, and pneumonia, among others. In addition to these immediate postoperative
complications, splenectomy itself is known to confer long‐term susceptibility to infection, sepsis, thrombosis, and other sequelae. Our goal was to identify factors that could prompt early investigation and treatment of both infectious and major complications.”
Efficacy of stapler versus hand-sewn closure after distal pancreatectomy (DISPACT)
“Resections of the pancreas reaching to the left of the superior mesenteric vein are defined as distal pancreatectomy. Most distal pancreatectomies are done electively (84%) as a result of chronic pancreatitis (24%), other benign diseases (22%), malignant diseases (18%), neuroendocrine tumours (14%), and pancreatic pseudocysts (6%). The remaining 16% are emergency cases after abdominal trauma or miscellaneous pathological
diagnoses. A systematic review supports the evidence that postoperative pancreatic fistula formation represents a major source of postoperative morbidity (13–64%) and is associated with several further complications, such as intra-abdominal abscess, wound infection, sepsis, malabsorption, and haemorrhage.
A meta-analysis of the most favoured and reported techniques (stapler trans-section and closure vs scalpel trans-section and hand-sewn closure of the pancreatic remnant) did
not define the optimum surgical technique of pancreatic stump closure. Therefore, the multicentre randomised DISPACT trial was designed to assess the effect of stapler
versus hand-sewn closure on formation of postoperative pancreatic fistula after distal pancreatectomy.”
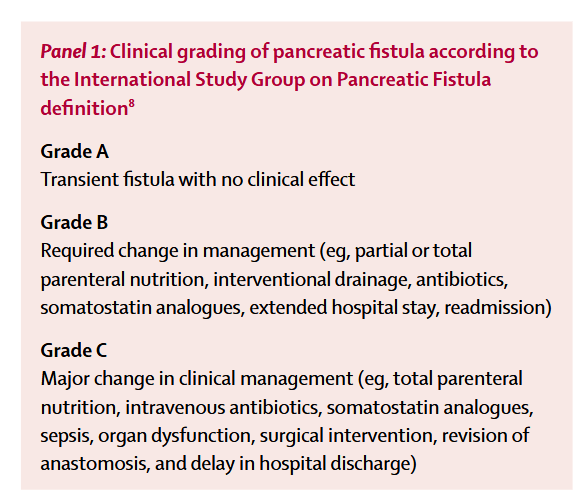
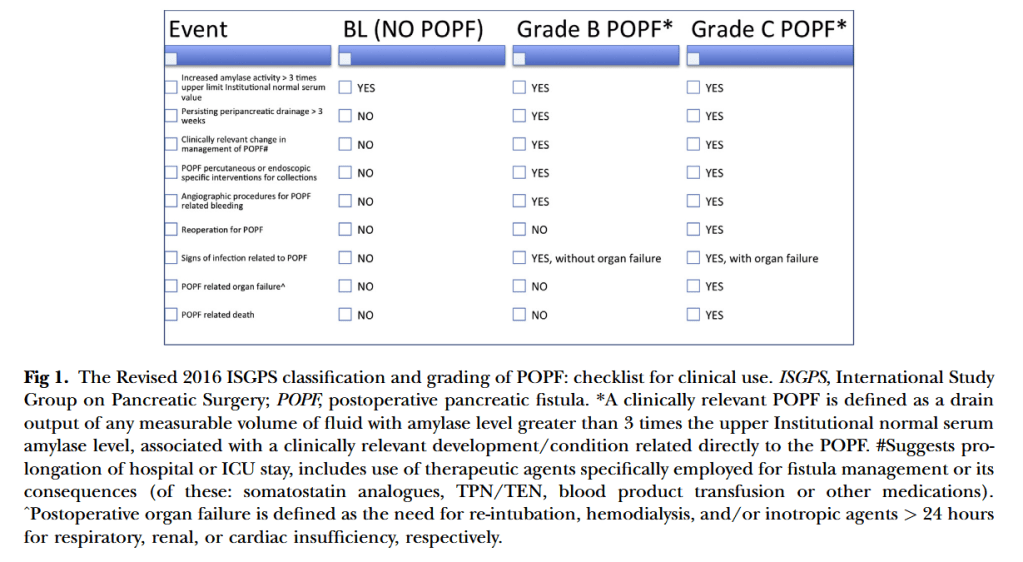
2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula
“Eleven years after its definition, postoperative pancreatic fistula (POPF) still remains one of the most harmful complications after pancreatic resection. Despite all the advances and technical modifications developed during this past decade to prevent POPF, the incidence of this dreaded complication still ranges between 3–45 % of pancreatic operations at high-
volume centers. Updating the ISGPF classification is both relevant and clinically important,
because POPF remains the single main determinant of serious postoperative morbidity and mortality related to pancreatic resection and plays a major role in terms of operation-related mortality, morbidity, hospital stay, and economic impact.”
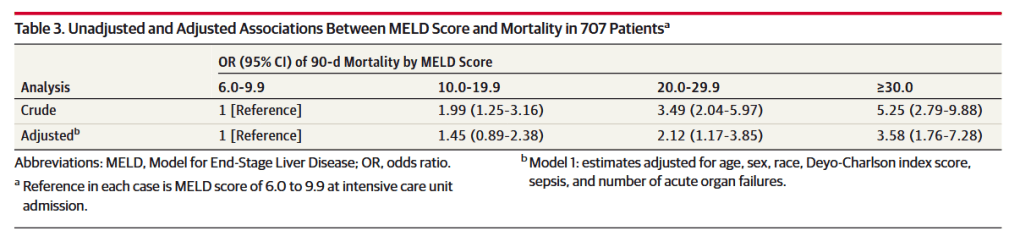
Association of Model for End-Stage Liver Disease Score With Mortality in Emergency General Surgery Patients
“Emergency general surgery (EGS) is associated with increased rates of morbidity and mortality compared with non-emergent general surgery cases.8 Patients undergoing EGS are approximately 2.5 times more likely to experience a significant complication and have a 6-fold increase in mortality relative to non-EGS patients. The underlying causes of this increased morbidity and mortality are not fully understood, but medical comorbidities and physiological derangements are likely to be contributing factors. Although surgical risk calculation tools such as the American College of Surgeons National Surgical Quality Improvement Project Surgical Risk Calculator are used to gain an objective sense of surgical risk stratification, such tools have yet to be comprehensively studied in this patient population and do not include the use of liver disease–specific assessment tools such as the MELD score in the prediction of outcomes among patients with CLD undergoing EGS.”