Wu Z, Zhou J, Pankaj P, Peng B. Comparative treatment and literature review for laparoscopic splenectomy alone versus preoperative splenic artery embolization splenectomy. Surg Endosc. 2012 Oct;26(10):2758-66.
Full-text for Emory users.
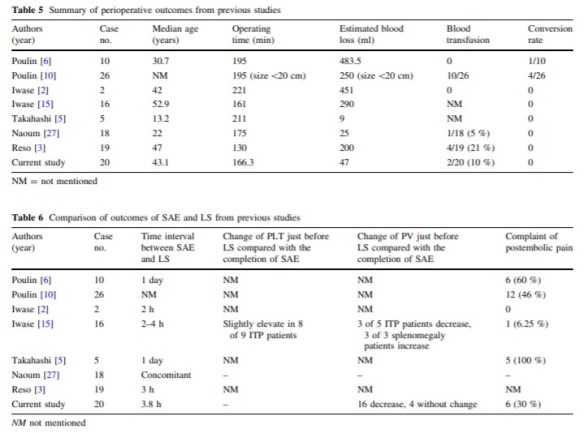
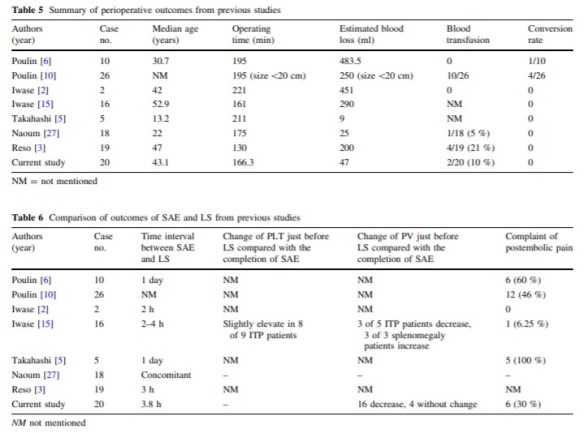
Results: Preoperative splenic artery embolization plus laparoscopic splenectomy was successfully performed in all patients in group 1. One patient in group 2 required an intraoperative conversion to traditional open splenectomy because of severe blood loss. Compared with group 2, significantly shorter operating time, less intraoperative blood loss, and shorter postoperative hospital stay were noted in group 1. No marked significant differences in postoperative complications of either group were observed. Compared with group 3, group 1 had less intraoperative blood loss, shorter postoperative stay, and fewer complications. No significant differences were found in operating time. There was a marked increase in platelet count and white blood count in both groups during the follow-up period.
Conclusions: Preoperative splenic artery embolization with laparoscopic splenectomy reduced the operating time and decreased intraoperative blood loss when compared with laparoscopic splenectomy alone or open splenectomy. Splenic artery embolization is a useful intraoperative adjunctive procedure for patients with splenomegaly because of the benefit of perioperative outcomes.
Continue reading →