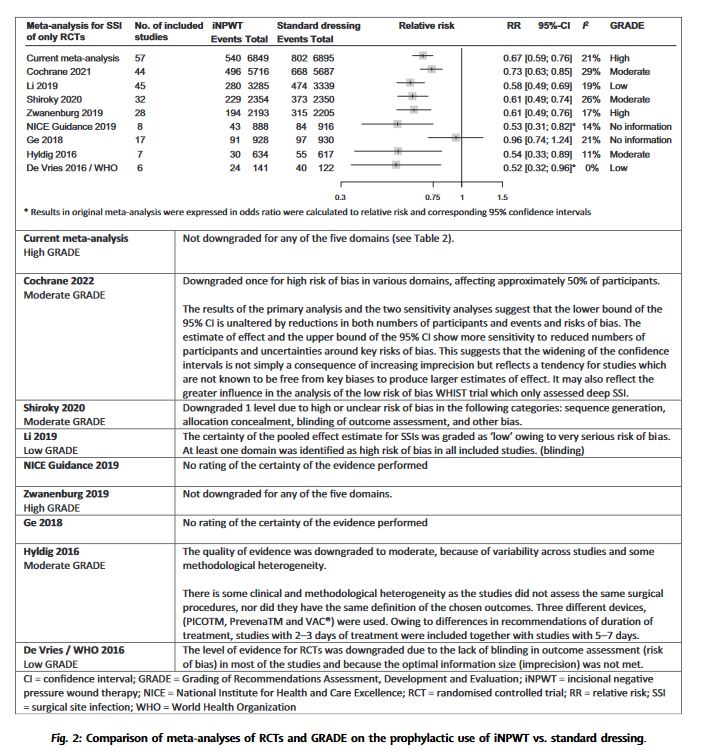
“The evidence on prophylactic use of negative pressure wound therapy on primary closed incisional wounds (iNPWT) for the prevention of surgical site infections (SSI) is confusing and ambiguous. Implementation in daily practice is impaired by inconsistent recommendations in current international guidelines and published meta-analyses. More recently, multiple new randomised controlled trials (RCTs) have been published. This study aimed to provide an overview of all meta-analyses and their characteristics; to conduct a new and up-to-date systematic review and meta-analysis and Grading of Recommendations Assessment, Development and Evaluation (GRADE) assessment; and to explore the additive value of new RCTs with a trial sequential analysis (TSA).”