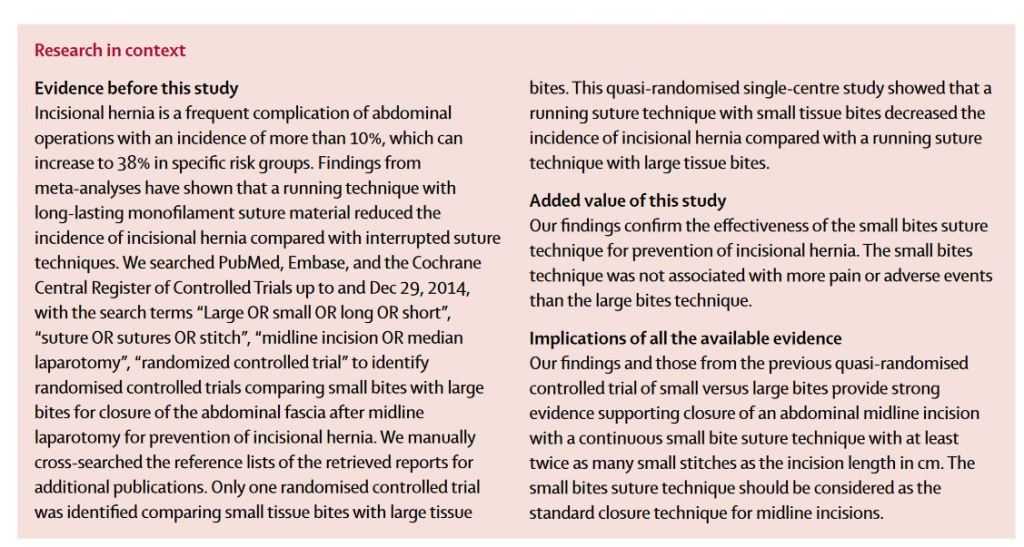
“Incisional hernia is a frequent complication of abdominal operations with an incidence of 10–23%, which can increase to 38% in specific risk groups. In the USA 4 million to 5 million laparotomies are done annually, suggesting that at least 400 000–500 000 incisional hernias can be expected to occur every year. Incisional hernia is associated with pain and discomfort, resulting in a decreased quality of life. Moreover, incarceration and strangulation of abdominal contents can take place, for which emergency surgery is indicated, with associated morbidity and mortality. About 348 000 operations for incisional hernia are done every year in the USA with US$3·2 billion in annual associated costs. Prevention of
incisional hernia is therefore of paramount importance.”