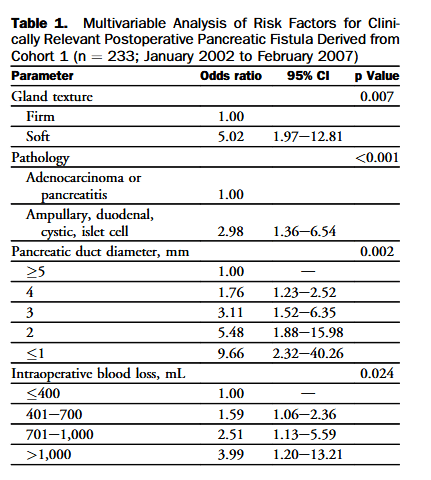
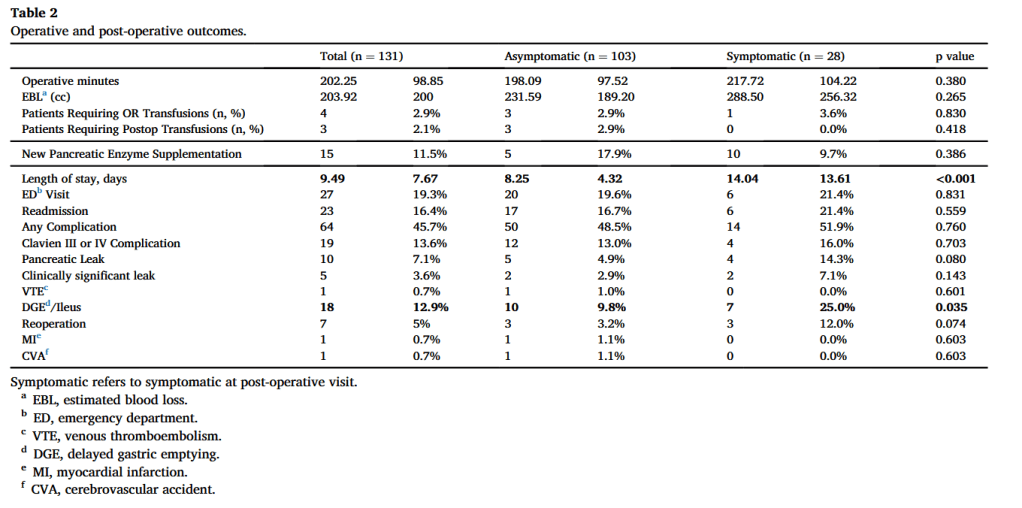
“Despite advancements in operative technique and improvements in postoperative outcomes, pancreatic fistula is widely considered to be the most common and
troublesome complication after pancreatic resection. It represents the factor most often linked with postoperative mortality, certain complications such as delayed gastric emptying, longer hospital stays, readmissions, and increased costs. Furthermore, it frequently delays
timely delivery of adjuvant therapies, and reduces overall patient survival. Placement of pancreatic duct stents, the use of somatostatin analogs or adhesive sealants, or modifications in reconstruction technique have done little to change the incidence or alter the impact of postoperative pancreatic fistulas (POPF).”