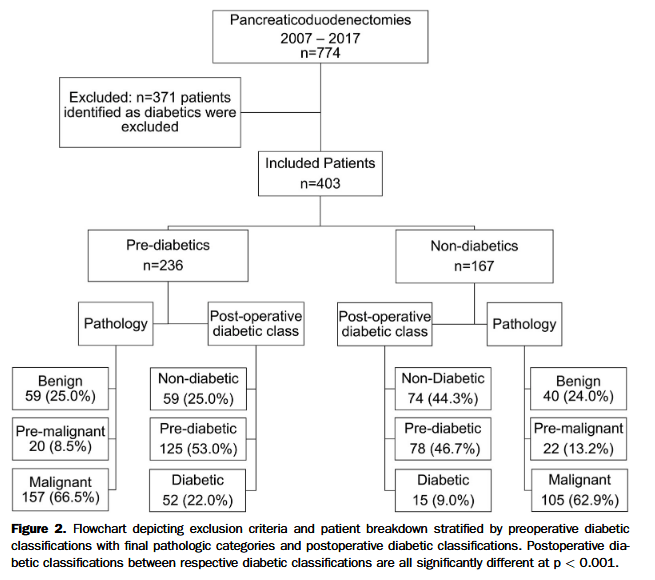
“The association with new-onset impaired glucose tolerance (or pre-diabetes) and diabetes has been observed since the inception of and subsequent popularization of pancreaticoduodenectomy (PD) the gold-standard surgical treatment for resectable pancreatic head pathologies. Standardization of surgical techniques, advancements in peri-operative care, and improved understanding of inflicting pathologies have led to drastic reductions in mortality and morbidity across all indications. Despite these advancements, the relationship between diabetes development and parenchymal resection, pathology, and
comorbid states remains understudied.”