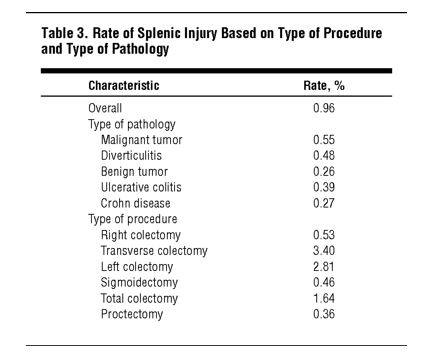
“Splenic injury is a major intraoperative complication of abdominal surgery and places patients at a higher risk of morbidity and mortality, of longer operating time, and of longer hospital stay. Splenic injuries may be managed nonoperatively or by splenorrhaphy, partial splenectomy, or complete splenectomy. Because splenectomy is reported to have higher mortality rates than splenorrhaphy, great effort is taken to preserve the spleen; however, excessive blood loss can mandate splenectomy.”